The integration of robotics into healthcare has transformed the surgical landscape, offering unparalleled precision, consistency, and minimally invasive solutions. The Role of Robotics in Modern Surgery extends far beyond technological novelty—it represents a significant leap forward in how surgeons perform complex procedures and how patients experience recovery.
In just two decades, robotic-assisted systems have evolved from experimental tools into indispensable assets in operating rooms worldwide. From cardiac to gynecologic procedures, robotics are reshaping surgical standards by enhancing visualization, dexterity, and control while reducing trauma to the patient.
This article explores how robotic surgery works, its applications, benefits, limitations, and what the future may hold for this rapidly advancing field.
What Is Robotic Surgery?
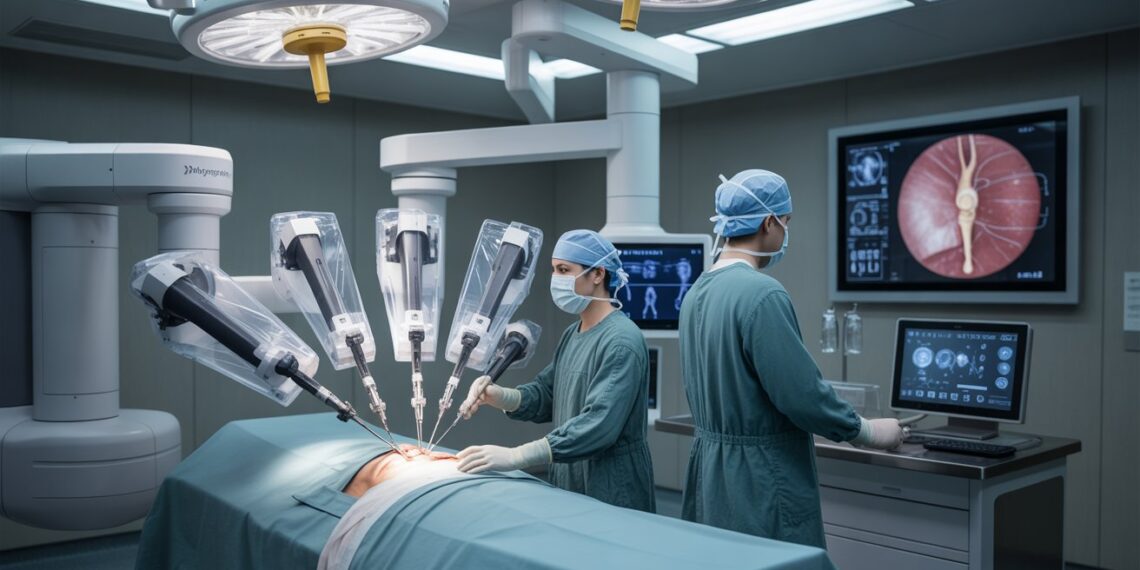
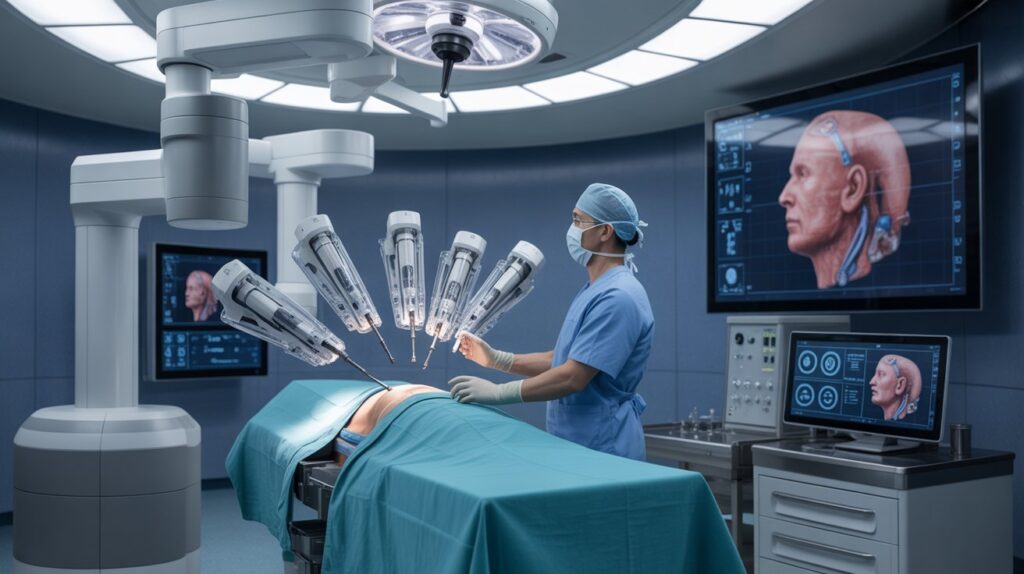
Robotic surgery, also known as robot-assisted surgery, allows surgeons to perform intricate operations using a combination of advanced robotic arms, miniature instruments, and high-definition cameras. The surgeon controls these instruments from a console that provides a magnified, three-dimensional view of the surgical site.
Unlike fully automated systems, robotic surgery is not performed by robots independently—the surgeon remains in complete control throughout the procedure. The robot functions as a precision extension of the surgeon’s hands, eliminating natural tremors and allowing for greater accuracy in confined spaces.
Common robotic systems include the da Vinci Surgical System, widely adopted across hospitals globally, as well as newer platforms designed for orthopedics, spine, and microsurgery.
How Robotic Surgery Works: Key Components
Robotic surgical systems typically consist of three major components:
-
Surgeon console: Where the surgeon sits and controls the robotic arms using joysticks and foot pedals. The console offers a 3D, high-definition visualization of the operative field.
-
Patient-side cart: Houses multiple robotic arms that hold surgical instruments and the camera.
-
Vision system: Provides real-time, magnified images that allow for superior precision and depth perception.
Through micro-movements and enhanced imaging, the robotic system translates the surgeon’s hand motions into smaller, more precise instrument actions inside the patient’s body.
Common Applications of Robotic Surgery
Today, robotic-assisted surgery spans multiple medical specialties. Some of the most common applications include:
Urology
Procedures such as prostatectomy and kidney surgeries benefit from robotics due to the confined anatomical spaces and need for nerve-sparing precision.
Gynecology
Robotic systems are used for hysterectomies, myomectomies, and endometriosis resections, reducing recovery time and blood loss.
General Surgery
Robotic technology is now applied to hernia repairs, gallbladder removals, and colorectal surgeries, improving ergonomics and surgical reach.
Cardiac and Thoracic Surgery
Surgeons utilize robotics for valve repair and coronary artery bypass procedures, where minimal invasiveness is essential to reduce postoperative pain and complications.
Orthopedic and Spine Surgery
Navigation-assisted robots help achieve precise implant placement, reducing the risk of alignment errors and improving functional outcomes.
Benefits of Robotic-Assisted Surgery
The rise of robotic surgery is driven by measurable improvements in outcomes and patient experience. Below are the primary benefits:
1. Enhanced Precision
The robotic system filters out tremors and enables delicate manipulation, allowing for precise movements even in tight anatomical regions.
2. Reduced Blood Loss and Scarring
Because incisions are smaller and tissue handling is gentler, patients experience less bleeding, minimal scarring, and reduced postoperative discomfort.
3. Shorter Recovery Time
Minimally invasive techniques translate into quicker mobilization, shorter hospital stays, and faster return to normal activity.
4. Improved Visualization
High-definition, 3D magnification provides superior visualization of nerves, vessels, and tissues—crucial for avoiding complications.
5. Ergonomic Advantages for Surgeons
The console design reduces fatigue during long surgeries and improves the surgeon’s comfort and focus.
Clinical studies have shown that, in many cases, robotic-assisted procedures achieve equivalent or better results compared to traditional laparoscopic or open approaches, particularly in precision-dependent surgeries.
Risks and Limitations
Despite its advantages, robotic surgery is not without challenges.
Learning Curve
Surgeons require specialized training and experience to fully utilize the technology’s capabilities. Institutions with high procedural volumes tend to have better outcomes.
Cost and Accessibility
The high purchase and maintenance cost of robotic systems can limit access, particularly in smaller hospitals or developing regions.
Longer Operating Times
Early in a surgeon’s experience, robotic procedures may take longer due to setup and docking times.
Technical Dependence
As with any technology, there’s a small risk of system malfunction, although redundant safety features minimize this possibility.
Understanding both the benefits and limitations helps patients make informed decisions and ensures that robotic surgery remains a tool for enhancement rather than replacement of surgical expertise.
Who Is an Ideal Candidate?
Not every patient or procedure is suitable for robotic surgery. Candidacy depends on several factors, including:
-
The type of surgery required
-
The patient’s overall health and anatomy
-
The surgeon’s training and institutional capabilities
Generally, robotic-assisted procedures are best suited for patients seeking minimally invasive solutions for conditions where precision and visualization are crucial. Discussing these aspects with a qualified surgeon is essential before deciding on a robotic approach.
Technology Behind Surgical Robotics
Robotic surgery integrates multiple advanced technologies:
Motion Scaling and Tremor Filtration
Transforms large hand movements into microscopic instrument actions, eliminating unintentional shaking.
Haptic Feedback
Emerging systems now provide tactile sensation, allowing surgeons to “feel” tissue resistance virtually.
Artificial Intelligence and Automation
AI algorithms are being developed to assist in real-time decision-making, suturing, and camera positioning, although human oversight remains mandatory.
Telepresence and Remote Surgery
With high-speed data networks, surgeons may eventually perform procedures remotely, providing access to specialized care in underserved regions.
The continued development of AI and sensor integration indicates that future systems will become more intuitive and partially autonomous—always under surgeon supervision.
Evidence and Clinical Outcomes
Robotic-assisted surgery has been widely studied across multiple specialties. Systematic reviews and meta-analyses suggest:
-
Comparable or superior oncological outcomes in prostate and gynecologic cancers
-
Reduced blood loss and postoperative pain
-
Shorter hospital stays in colorectal and bariatric surgeries
-
No significant increase in complication rates when performed by experienced surgeons
While robotic systems improve precision, evidence also highlights the importance of surgeon experience and institutional support in achieving optimal results. The technology amplifies skill—it does not replace it.
Costs, Access, and Global Adoption
The financial aspect remains one of the biggest barriers to widespread adoption. Robotic platforms can cost over $1 million to install, with ongoing maintenance and instrument replacement expenses.
However, global trends indicate steady growth. Health systems in North America, Europe, and Asia are expanding their robotic capabilities, with newer, more cost-efficient platforms entering the market. In some countries, national health systems are investing in robotics to improve long-term efficiency and patient throughput.
As technology matures and competition increases, costs are expected to decline, making robotic surgery more accessible worldwide.
Future Directions: Where Surgical Robotics Is Heading
The next decade promises even greater innovation. Anticipated developments include:
-
Smaller, modular robotic systems that can be easily adapted for different procedures
-
AI-guided image recognition to assist in identifying anatomy and pathology in real time
-
Haptic-enabled consoles for improved tactile feedback
-
Remote and telesurgery capabilities connecting specialists with distant hospitals
-
Integration with augmented and virtual reality for training and intraoperative navigation
These advances will continue to expand the role of robotics in modern surgery, creating new possibilities for precision, safety, and global healthcare access.
Patient Considerations: Questions to Ask Your Surgeon
If you’re considering robotic surgery, use this checklist to guide your consultation:
-
How many robotic procedures have you performed?
-
What are the potential benefits and risks specific to my condition?
-
How does robotic surgery compare to laparoscopic or open surgery for my case?
-
What is the expected recovery timeline?
-
What happens if the robotic system encounters a technical issue?
-
What are the total costs, and does insurance cover it?
Informed discussions help ensure patients choose the safest and most effective approach for their unique medical needs.
Frequently Asked Questions (FAQs)
What is robotic surgery?
Robotic surgery is a minimally invasive technique where surgeons use computer-controlled robotic arms to perform operations through small incisions with enhanced precision.
Is robotic surgery safer than traditional surgery?
In many procedures, robotic surgery offers equal or improved safety due to better visualization and precision, though outcomes depend on surgeon expertise and patient factors.
Does the robot perform surgery on its own?
No. The surgeon controls all movements from a console. The robot functions as an extension of the surgeon’s hands, not an autonomous operator.
How long does recovery take after robotic surgery?
Recovery time varies by procedure, but most patients experience shorter hospital stays and faster return to normal activities compared to traditional surgery.
What are the limitations of robotic surgery?
High costs, limited availability, and the need for specialized training are current limitations. Additionally, not all procedures are suitable for robotic assistance.
What is the future of robotic surgery?
Future innovations will likely include AI assistance, haptic feedback, and remote surgical capabilities, expanding accessibility and precision in medical care.
Conclusion
The Role of Robotics in Modern Surgery continues to redefine what is possible in the operating room. Through improved precision, smaller incisions, and faster recovery, robotic systems empower surgeons and benefit patients across numerous specialties.
Yet, technology alone is not the solution—its true potential lies in skilled hands, continuous training, and ethical implementation. As costs decrease and innovation accelerates, robotic-assisted surgery is poised to become the global standard for minimally invasive care.
By understanding both its strengths and limitations, patients and healthcare professionals can make informed choices and fully embrace this transformative evolution in modern medicine.