Healthcare has always been about timely information and quick interventions. For decades, patients had to visit hospitals or clinics for every checkup, no matter how small. This model often meant delays in diagnosis, missed warning signs, and costly hospital readmissions. But things are changing.
The rise of digital health tools has made it possible to track patients’ vital signs and chronic conditions in real time, even when they are hundreds of miles away from their doctors. This is where Remote Patient Monitoring (RPM) steps in.
This article — Remote Patient Monitoring Explained — provides a complete, in-depth look at how RPM works, the technology behind it, its benefits and limitations, current global adoption, and what the future may hold. By the end, you’ll understand why RPM is seen as one of the most transformative trends in modern healthcare.
What is Remote Patient Monitoring?
Remote Patient Monitoring (RPM) refers to a system in which healthcare providers use connected medical devices and digital platforms to monitor patients’ health conditions outside traditional hospital or clinic settings.
The goal is simple yet powerful: to bring healthcare into patients’ daily lives instead of restricting it to scheduled appointments.
Example: Diabetes Care
Instead of a patient with diabetes waiting for quarterly blood sugar reviews, RPM allows daily glucose readings to be transmitted directly to their provider. If blood sugar spikes dangerously, an alert can be generated instantly, prompting timely intervention.
Defining Characteristics
-
Continuous or scheduled monitoring instead of sporadic check-ins.
-
Device-based data collection (blood pressure cuffs, glucometers, etc.).
-
Secure digital transmission of health data to providers.
-
Provider oversight and intervention, when needed.
-
Integration with EHRs for holistic patient profiles.
Remote Patient Monitoring Explained vs. Other Digital Health Approaches
It’s easy to confuse RPM with other virtual health terms, but there are important differences.
-
Telehealth: A broad umbrella term that includes all remote healthcare services, from video calls to mobile health apps.
-
Telemedicine: Refers specifically to remote clinical consultations between providers and patients.
-
Remote Therapeutic Monitoring (RTM): Focuses on adherence and response to therapy (e.g., physiotherapy exercises).
-
RPM: Primarily about collecting, transmitting, and analyzing physiological data.
Think of it this way: Telemedicine connects patients and doctors through conversations, while RPM connects them through data.
How Remote Patient Monitoring Works
The effectiveness of RPM depends on its seamless workflow.
Step 1: Device Allocation
Patients receive devices such as connected scales, ECG patches, or smart inhalers. These devices are usually easy to use, often requiring just a single button press.
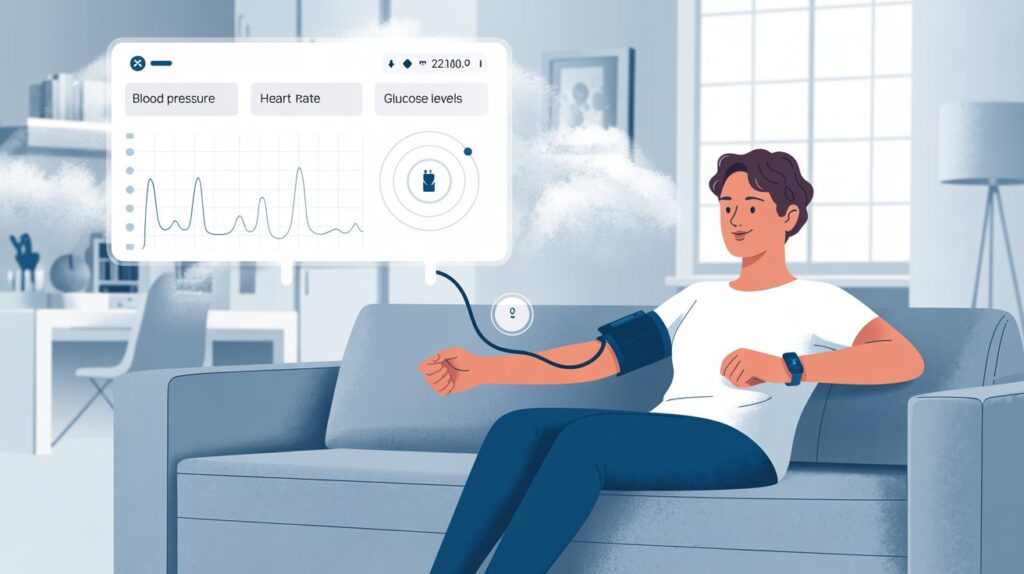
Step 2: Data Collection
The device measures metrics like blood pressure, blood sugar, oxygen saturation, or heart rhythm.
Step 3: Secure Transmission
Data is transmitted automatically via Bluetooth, Wi-Fi, or cellular networks to cloud-based platforms.
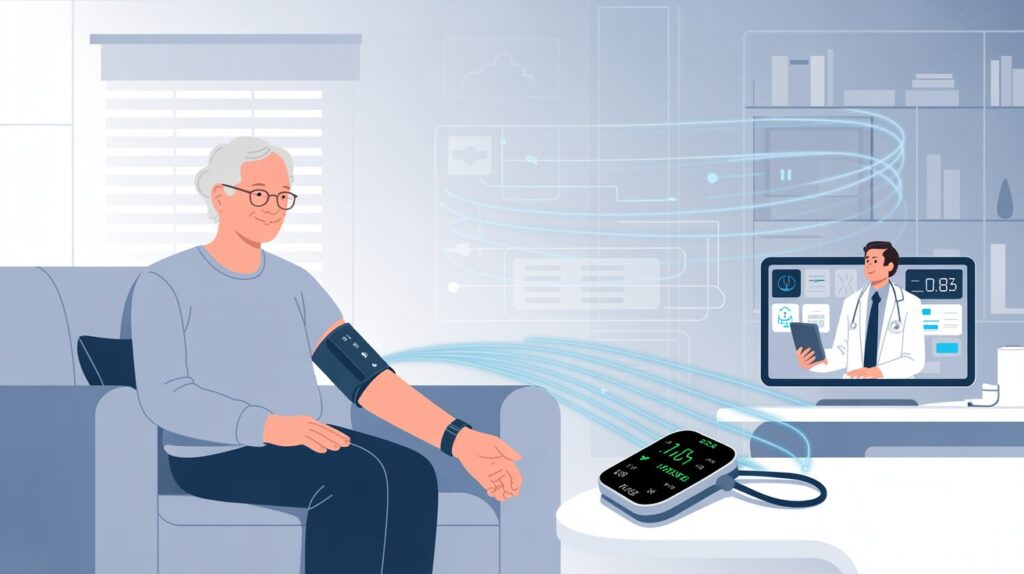
Step 4: Provider Review
Healthcare teams receive the data on dashboards, often integrated with electronic health records. Abnormal readings trigger alerts.
Step 5: Intervention
Providers can reach out via calls, messages, or telehealth visits to adjust treatment, prescribe medication, or recommend hospitalization.
Common Devices in RPM
-
Cardiac monitoring devices (wearable ECG, Holter monitors)
-
Glucose monitors (finger-stick or continuous)
-
Pulse oximeters (oxygen saturation, especially critical in respiratory illness)
-
Weight scales (used in heart failure monitoring)
-
Smart inhalers (track medication adherence in asthma/COPD)
-
Blood pressure monitors
-
Activity trackers and wearables (Fitbit, Apple Watch with ECG features)
Applications of Remote Patient Monitoring
RPM has applications across nearly all branches of healthcare.
1. Chronic Disease Management
-
Diabetes: Continuous glucose monitoring (CGM) helps reduce complications. Studies show RPM users achieve better HbA1c control.
-
Hypertension: Remote blood pressure monitoring can lower cardiovascular risks by enabling timely medication adjustments.
-
Heart Failure: Daily weight tracking helps identify fluid retention early, preventing hospitalization.
2. Post-Operative Recovery
After surgery, patients can be monitored for infections, blood pressure stability, or irregular heart rhythms without staying in hospital unnecessarily.
3. Maternal and Fetal Monitoring
Pregnant women can be monitored for preeclampsia (high blood pressure), gestational diabetes, and fetal heart rates. This is especially helpful in rural areas where frequent visits may be difficult.
4. Elderly Care and Fall Prevention
Elderly patients living alone can use wearables that track activity and detect falls. This improves independence while ensuring safety.
5. Respiratory Illness Monitoring
For patients with COPD or post-COVID lung damage, RPM devices like pulse oximeters and spirometers help manage breathing difficulties.
6. Mental Health Integration
Though less common, wearable devices can track sleep and activity, offering insights for behavioral therapy.
Benefits of Remote Patient Monitoring
For Patients
-
Convenience: No need for frequent travel to hospitals.
-
Empowerment: Patients actively engage in their own care.
-
Better outcomes: Continuous monitoring enables earlier interventions.
-
Reduced anxiety: Patients feel safer knowing their providers are monitoring them.
For Providers
-
Real-time data: More accurate than occasional clinic readings.
-
Operational efficiency: Less time spent on routine checkups.
-
Improved communication: Providers can contact patients proactively.
For Healthcare Systems
-
Lower costs: RPM reduces unnecessary emergency visits and readmissions.
-
Scalability: Systems can manage larger patient populations remotely.
-
Alignment with value-based care: Outcomes-focused reimbursement is easier with RPM data.
Case Study: Heart Failure Management
A large U.S. study found that heart failure patients using RPM experienced a 50% reduction in hospital readmissions compared to those receiving only traditional care.
Challenges and Barriers
Despite its benefits, RPM faces hurdles.
Technical Barriers
-
Device malfunction or inaccuracy can lead to false alarms.
-
Poor internet connectivity in rural areas hinders effectiveness.
-
Integration with hospital IT systems remains complex.
Patient Barriers
-
Not all patients are comfortable using technology.
-
Elderly patients may need additional training.
-
Privacy concerns discourage some from sharing data.
Provider Barriers
-
Initial setup costs for devices and platforms are high.
-
Staffing models must adapt to continuous monitoring.
-
Managing data overload is challenging — too many alerts can lead to “alarm fatigue.”
Regulations and Reimbursement
United States
-
Medicare recognizes RPM as reimbursable under CPT codes such as 99453 (setup), 99454 (data transmission), 99457 (clinical monitoring).
-
Private insurers increasingly follow Medicare’s lead.
Europe
-
GDPR sets strict requirements for patient data protection.
-
Countries like Germany have introduced Digital Health Applications (DiGA) that reimburse RPM.
Asia and Emerging Economies
-
Adoption is growing, especially with mobile-first solutions.
-
Barriers include lack of standardized reimbursement and regulatory frameworks.
Best Practices for Implementing RPM
Healthcare organizations can maximize success by following these steps:
-
Identify Patient Populations: Start with groups most likely to benefit (e.g., heart failure, diabetes).
-
Choose User-Friendly Devices: Simplicity is key for patient adoption.
-
Educate Patients: Training and ongoing support ensure compliance.
-
Integrate with EHRs: Data should flow seamlessly into provider dashboards.
-
Set Clear Protocols: Define thresholds for alerts, escalation procedures, and communication channels.
-
Monitor and Refine: Continuously evaluate outcomes, patient satisfaction, and cost savings.
The Future of Remote Patient Monitoring
Emerging Technologies
-
AI-powered predictive analytics: Algorithms can predict complications before they occur.
-
Next-gen wearables: Smaller, more accurate, and more comfortable sensors.
-
IoT integration: Smart homes with medical sensors embedded in everyday devices.
-
Virtual hospitals: Patients monitored entirely from home, reducing the need for physical hospital beds.
Market Outlook
-
Analysts predict the global RPM market will surpass $175 billion by 2030.
-
Growth is fueled by aging populations, rising chronic disease burden, and government incentives for digital health.
The Patient of the Future
Imagine an elderly patient with heart failure:
-
Their smart scale detects sudden weight gain, alerting the care team.
-
An AI algorithm predicts a risk of fluid overload.
-
The provider calls immediately, adjusting medication, preventing hospitalization.
This is not science fiction — it’s the direction healthcare is moving.
Frequently Asked Questions (FAQs)
1. What is Remote Patient Monitoring?
It is the use of connected devices to collect patient health data outside clinical settings and transmit it securely to providers.
2. How is RPM different from telehealth?
Telehealth covers all virtual healthcare interactions, while RPM focuses specifically on data-driven continuous monitoring.
3. Which conditions benefit most from RPM?
Chronic diseases like diabetes, hypertension, COPD, and heart failure benefit the most, along with elderly and post-surgical patients.
4. What are the biggest barriers?
Technical issues (device accuracy, connectivity), patient reluctance, and cost of implementation are key challenges.
5. Is Remote Patient Monitoring cost-effective?
Yes, RPM reduces hospital admissions, emergency visits, and complications, making it cost-saving in the long term.
6. Is patient data secure in RPM?
Most platforms comply with privacy regulations like HIPAA and GDPR, but providers must ensure encryption and proper consent practices.
Conclusion
Healthcare is undergoing a paradigm shift, moving away from hospital-centric models to patient-centered, data-driven care. RPM embodies this transformation by bridging the gap between clinic and home.
With its ability to improve outcomes, reduce costs, and empower patients, RPM is becoming a central pillar of modern healthcare systems worldwide. Although challenges remain — from technical integration to regulatory hurdles — the trajectory is clear.
In short, Remote Patient Monitoring Explained reveals a future where healthcare is not bound by physical walls but integrated seamlessly into patients’ daily lives. As technology advances, RPM will play an even greater role in predictive, preventive, and personalized medicine.