In the modern era of digital healthcare, technology is not just assisting clinicians — it’s redefining how they care for patients. One of the most impactful innovations driving this transformation is the use of Biometric Devices in Patient Monitoring. These devices have evolved beyond simple wearables into sophisticated tools capable of continuously tracking physiological and behavioral data, providing clinicians with real-time insights that can save lives.
As the global healthcare system shifts toward preventive care, remote patient monitoring (RPM), and personalized medicine, biometrics play a central role. From fingerprint and facial recognition to non-invasive sensors measuring heart rate, oxygen saturation, and electrocardiogram (ECG) signals, biometric technologies are revolutionizing how medical professionals assess patient health.
This article explores what biometric devices are, how they function in patient monitoring, their clinical applications, benefits, challenges, and the future of this rapidly growing field.
What Are Biometric Devices in Patient Monitoring?
Biometric devices are tools that measure, record, and analyze unique physiological or behavioral characteristics of an individual. In healthcare, these devices go beyond simple identification; they continuously capture health metrics such as pulse rate, temperature, blood pressure, or ECG signals, helping physicians monitor patient status both inside and outside hospital settings.
Common Biometric Parameters Measured
-
Physiological biometrics: Heart rate, respiratory rate, blood oxygen (SpO₂), blood glucose, skin temperature, ECG patterns, and blood pressure.
-
Behavioral biometrics: Gait analysis, voice patterns, and motion-based activity levels.
-
Identification biometrics: Fingerprint, facial, iris, or palm vein recognition for secure patient verification.
By combining identification and health data, Biometric Devices in Patient Monitoring create an ecosystem where accurate, continuous, and secure tracking of patients becomes a reality.
The Evolution of Biometric Monitoring in Healthcare
Originally, biometrics were used mainly for patient identification, preventing mix-ups in hospitals and ensuring accurate record-keeping. However, the introduction of Internet of Things (IoT) technologies, wearable sensors, and AI-driven analytics has expanded their use into real-time physiological monitoring.
From Manual Checks to Continuous Monitoring
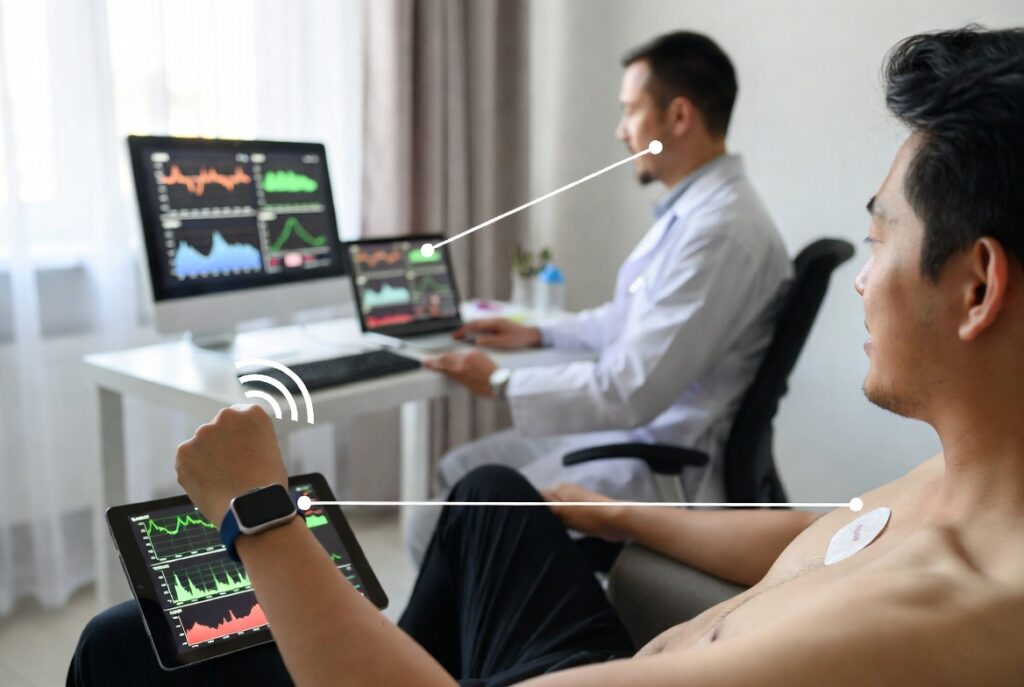
Traditional patient monitoring involved manual checks by nurses and periodic updates in medical charts. Biometric devices now automate these processes. Smart patches, wearable ECGs, and wireless vital-sign sensors provide constant data streams that are securely transmitted to healthcare dashboards.
Integration with Remote Patient Monitoring (RPM)
During the rise of telehealth, especially post-pandemic, biometric monitoring became a cornerstone of RPM. Patients recovering at home after surgery or living with chronic conditions can now be continuously monitored through wearable or implantable devices, reducing hospital readmissions and improving outcomes.
Types of Biometric Devices Used in Patient Monitoring
Biometric monitoring devices vary widely depending on their purpose, technology, and application. Below are the most common categories:
1. Wearable Biometric Sensors
These include smartwatches, wristbands, and chest patches that track parameters like heart rate, blood oxygen, and activity. They are typically lightweight, non-invasive, and ideal for continuous monitoring.
Examples:
-
ECG patches for arrhythmia detection
-
Pulse oximeters for oxygen saturation
-
Smartwatches with heart-rate and sleep tracking
2. Implantable and Ingestible Sensors
Implantable devices such as glucose monitors or pacemaker sensors track internal metrics more precisely. Ingestible sensors, though less common, can monitor medication adherence and digestive conditions.
3. Contactless Biometric Monitors
Advanced systems now include camera-based or radar sensors that detect vital signs without direct contact — a useful innovation for infection control in clinical environments.
4. Biometric Identification Devices
While not directly medical monitors, fingerprint or facial recognition devices play a crucial role in ensuring correct patient identification, reducing errors in medication delivery and electronic health records (EHRs).
How Biometric Devices Work in Patient Monitoring
Step 1: Data Capture
Sensors detect biometric data such as ECG patterns, heart rate, or body temperature using optical, electrical, or mechanical methods.
Step 2: Data Transmission
The data is transmitted wirelessly — often via Bluetooth, Wi-Fi, or 5G — to a centralized monitoring platform or the cloud.
Step 3: Data Analysis
Machine learning algorithms analyze these streams in real time to detect abnormalities, trends, or early warning signs.
Step 4: Clinical Decision Support
Physicians receive alerts or dashboards highlighting deviations from normal patterns, allowing them to intervene early, sometimes before symptoms become critical.
This integration of biometrics, cloud computing, and artificial intelligence forms the backbone of next-generation patient monitoring systems.
Benefits of Using Biometric Devices in Patient Monitoring
The healthcare industry is embracing biometrics for several compelling reasons. Below are the primary benefits:
1. Continuous, Real-Time Monitoring
Biometric devices enable 24/7 data collection, offering a continuous picture of a patient’s health rather than sporadic snapshots taken during office visits.
2. Early Detection and Intervention
By identifying changes in vital signs before symptoms escalate, clinicians can intervene sooner — potentially preventing hospitalizations or medical emergencies.
3. Enhanced Patient Engagement
Patients using wearable biometrics are often more involved in their care. Real-time feedback helps them understand their health trends, promoting better compliance.
4. Reduced Healthcare Costs
Remote biometric monitoring can reduce hospital stays, minimize readmissions, and optimize resource allocation.
5. Improved Accuracy and Security
Unlike manual readings, biometric data is less prone to human error. Biometric authentication also ensures that health records are securely linked to the correct patient.
Clinical Applications of Biometric Monitoring
1. Chronic Disease Management
Patients with diabetes, heart disease, or COPD benefit most from continuous biometric monitoring. Devices can alert clinicians to deviations that indicate exacerbations, enabling early interventions.
2. Postoperative and Rehabilitation Monitoring
Wearable biometric sensors track vital signs and mobility during recovery, providing clinicians with data that supports safer discharge and remote follow-up.
3. Mental Health and Sleep Disorders
Certain biometric parameters — such as heart rate variability or sleep cycles — provide insight into stress levels and mental well-being.
4. Elderly and Home Care
For aging populations, continuous biometric monitoring helps detect falls, irregular heart rhythms, or respiratory issues in real time, promoting independence and safety.
Integration with Cloud and AI Technologies
The power of Biometric Devices in Patient Monitoring is magnified by cloud connectivity and artificial intelligence.
-
Cloud Platforms: Enable scalable storage and remote access for clinicians and healthcare systems.
-
AI Algorithms: Detect anomalies faster than manual analysis, learning from patient data to improve prediction accuracy.
-
Edge Computing: Reduces latency by processing data locally on the device before sending summaries to the cloud.
For instance, platforms built on architectures like AWS or Azure can process vast biometric data sets while maintaining strict compliance with healthcare privacy standards (HIPAA, GDPR).
Privacy, Security, and Ethical Considerations
While biometric monitoring brings immense benefits, it also introduces new challenges around data privacy and ethics.
Data Ownership and Consent
Patients must give informed consent for how their biometric data is collected, used, and shared. Transparency about storage, access, and retention policies is essential.
Security and Encryption
Biometric data is highly sensitive. Devices and cloud systems must employ robust encryption protocols, multi-factor authentication, and secure APIs to prevent breaches.
Regulatory Compliance
Manufacturers must ensure compliance with frameworks such as the FDA’s medical device regulations, ISO standards, and national privacy laws.
Healthcare providers implementing biometric systems should also undergo regular cybersecurity audits and maintain strong governance policies to protect patient data integrity.
Challenges in Adopting Biometric Monitoring Systems
-
Data Overload: Continuous data streams can overwhelm clinicians without proper filtering or AI triage.
-
Integration Barriers: Many hospitals struggle to integrate biometric data into legacy electronic health records (EHRs).
-
Cost of Implementation: High-quality sensors and cloud infrastructure can be costly upfront, especially for smaller healthcare systems.
-
User Comfort and Adherence: Patients may resist wearing certain devices long-term due to discomfort or privacy concerns.
-
Standardization Issues: The lack of universal data formats and validation criteria complicates interoperability between device manufacturers.
Despite these challenges, adoption continues to grow rapidly, driven by proven clinical and economic outcomes.
Future of Biometric Devices in Patient Monitoring
The future of biometrics in healthcare is promising and innovation-driven. Emerging trends include:
-
Multimodal Biometric Systems: Combining multiple biometric parameters (e.g., ECG + PPG + motion) for greater accuracy.
-
Contactless Monitoring: Cameras and radar sensors capable of reading pulse and respiration remotely.
-
AI Predictive Analytics: Advanced algorithms predicting cardiac arrest or infection risk before clinical symptoms appear.
-
Integration with Electronic Health Records (EHR): Seamless interoperability enabling full patient visibility across care teams.
-
Personalized Healthcare Models: Tailoring treatment plans based on continuous biometric insights.
As technology advances, the boundaries between healthcare and everyday life will blur, with biometric monitoring becoming an integral part of preventive medicine and chronic care.
FAQs About Biometric Devices in Patient Monitoring
1. What are biometric devices used for in patient monitoring?
They continuously measure physiological signals like heart rate, oxygen saturation, and temperature to track patient health in real time, supporting early diagnosis and remote care.
2. Are biometric monitoring devices safe to use?
Yes, most FDA-approved biometric devices undergo strict validation and clinical testing to ensure safety and accuracy when used as directed.
3. How do biometric devices transmit patient data?
They typically use wireless protocols like Bluetooth or 5G to send encrypted data to cloud platforms or clinical dashboards, ensuring secure, real-time access.
4. Can biometric monitoring improve patient outcomes?
Absolutely. Studies show that continuous biometric monitoring can reduce hospital readmissions, detect early warning signs, and improve chronic disease management.
5. What are the privacy concerns with biometric data?
Privacy issues include unauthorized access, misuse of biometric templates, and unclear consent policies. Strong encryption and transparent governance are vital for compliance.
Conclusion
Biometric Devices in Patient Monitoring represent one of the most significant technological leaps in modern healthcare. They enable clinicians to shift from reactive care to proactive and preventive care, improving patient outcomes while optimizing system efficiency.
By combining continuous biometric data with AI-driven analytics, healthcare providers can detect health issues earlier, engage patients more effectively, and deliver truly personalized care. However, success depends on balancing innovation with strict privacy, security, and ethical standards.
As the healthcare landscape continues to evolve, biometrics will remain at the heart of connected, intelligent, and patient-centered care — transforming not only how patients are monitored but how they are ultimately healed.