As of 2026, electronic medical record (EMR) systems are no longer just digital filing cabinets. They have evolved into clinical intelligence platforms that influence care quality, physician workload, reimbursement accuracy, and even patient outcomes.
Clinics today face new pressures:
-
Higher patient volumes with fewer clinicians
-
Value-based care models replacing fee-for-service
-
AI documentation tools reshaping daily workflows
-
Stricter data-sharing and interoperability expectations
Choosing the right EMR system in 2026 directly affects whether a clinic scales smoothly or burns out staff and leaks revenue.
This guide goes beyond surface-level feature lists. It explains how modern EMRs actually perform in real clinical environments, compares leading platforms, and highlights 2026 trends that most reviews still ignore.
Why EMR Selection Matters More in 2026 Than Ever
Recent healthcare IT studies (2024–2025) show that clinics using poorly aligned EMR systems experience:
-
Up to 27% longer documentation time per visit
-
Higher clinician burnout scores
-
Increased claim denials due to coding mismatches
-
Lower patient satisfaction from portal friction
Meanwhile, clinics using workflow-aligned EMRs report:
-
Faster chart completion
-
More accurate coding
-
Higher patient engagement through portals and messaging
-
Better performance under value-based contracts
The difference is no longer “digital vs paper.”
It’s intelligent EMR vs administrative burden.
EMR vs EHR in 2026: The Practical Difference Clinics Should Know
While the terms are often used interchangeably, the distinction still matters in practice.
EMR (Electronic Medical Record):
-
Primarily clinic-centric
-
Optimized for day-to-day documentation, scheduling, and billing
-
Faster to deploy, often more customizable
-
Ideal for independent clinics and specialty practices
EHR (Electronic Health Record):
-
Designed for cross-organization data sharing
-
Common in hospitals and health systems
-
Heavier compliance and interoperability layers
-
Often higher cost and complexity
2026 Reality:
Many top “EMRs” now include EHR-level interoperability, blurring the line. Clinics should focus less on labels and more on actual data exchange capability (FHIR, HL7, API access).
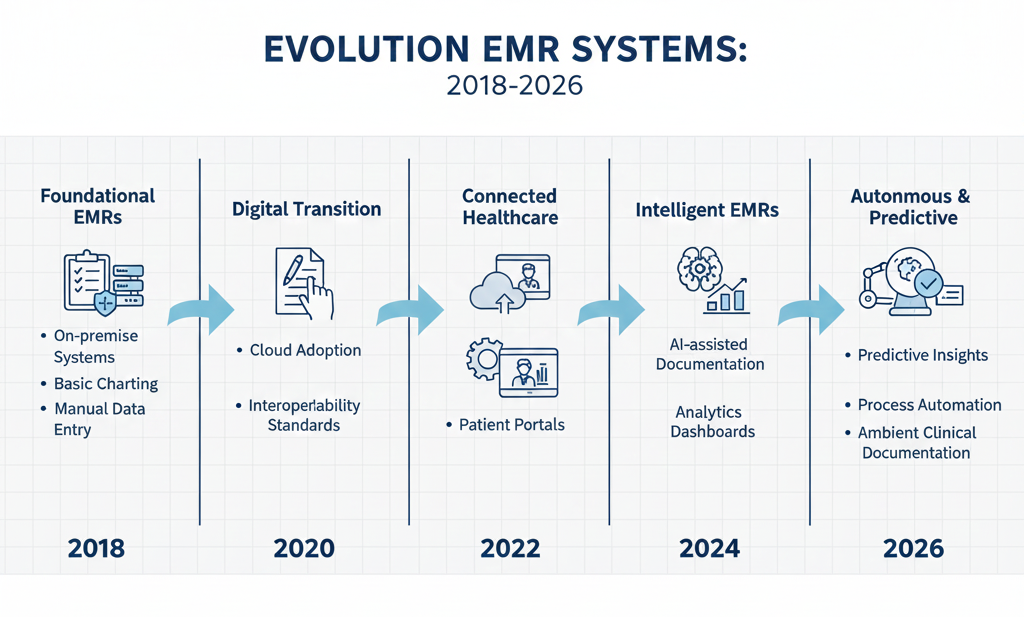
What Has Changed in EMR Systems (2024–2026)
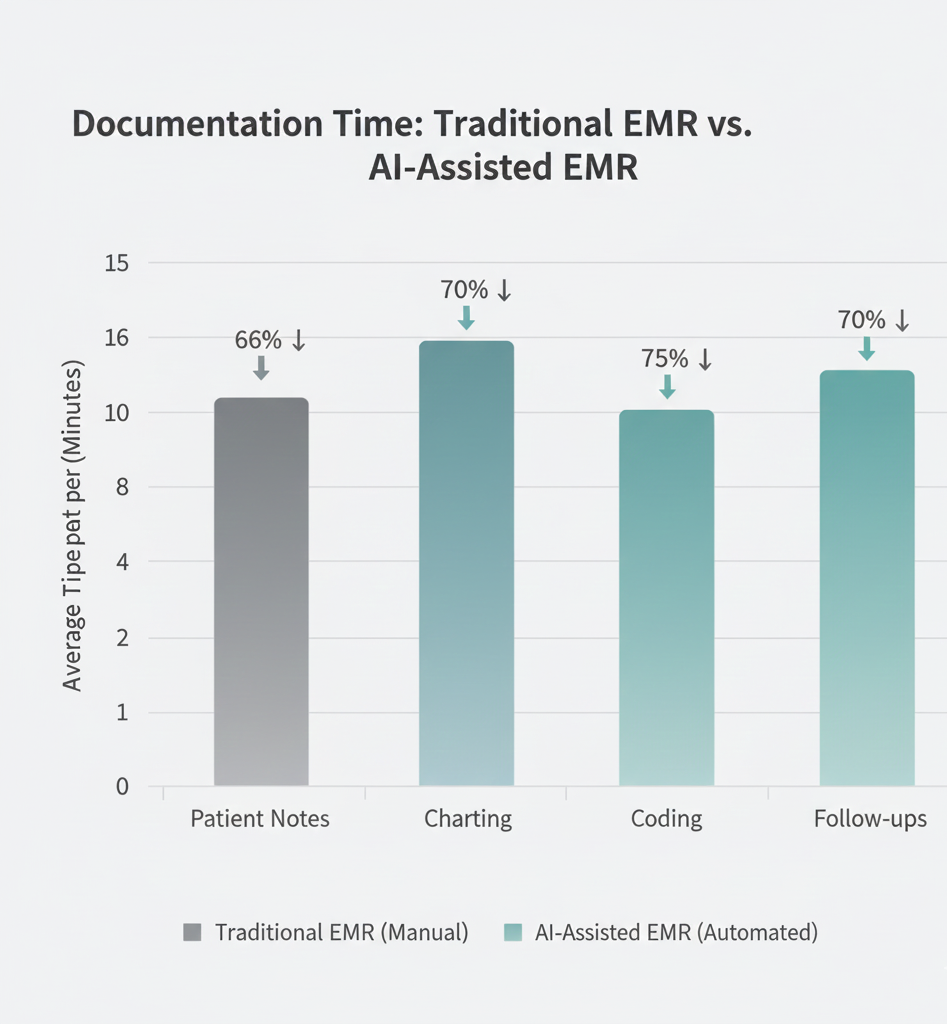
1. AI-Assisted Documentation Is No Longer Optional
Modern EMRs increasingly include:
-
Ambient clinical note generation
-
Smart summaries of patient history
-
Automated coding suggestions
Clinics using AI-assisted charting report 15–30% reduction in after-hours documentation.
2. Interoperability Is Actively Enforced
New regulatory pressure means EMRs must:
-
Support real-time data sharing
-
Allow patient-controlled data access
-
Integrate with labs, imaging, and pharmacies seamlessly
3. Revenue Cycle Intelligence Is Embedded
EMRs now flag:
-
Under-coded visits
-
Missing documentation
-
High denial-risk claims before submission
This directly improves cash flow not just compliance.
Best EMR Systems for Clinics in 2026 (In-Depth Review)
Epic Systems
Best for: Large clinics, multi-location practices, specialty groups
Why Epic Works in 2026
Epic’s strength is ecosystem depth. Clinics benefit from:
-
Advanced population health analytics
-
Deep interoperability with hospitals
-
AI-driven clinical decision support
Where Epic Struggles
-
High cost
-
Long implementation timelines
-
Overkill for small clinics
Expert Take:
Epic is powerful, but only worth it if your clinic needs enterprise-grade scale and integration.
Oracle Health (Cerner)
Best for: Mid-to-large clinics prioritizing cloud infrastructure
Oracle’s acquisition of Cerner has accelerated:
-
Cloud migration
-
Predictive analytics
-
Interoperability investments
Strengths
-
Strong data analytics
-
Scalable architecture
-
Improved reporting since Oracle integration
Limitations
-
Interface learning curve
-
Customization can be complex
eClinicalWorks
Best for: Small to mid-size independent clinics
Why Clinics Choose It
-
Specialty-specific templates
-
Affordable pricing model
-
Built-in telehealth and patient engagement
2026 Advantage
-
AI tools for documentation and coding
-
Improved patient portal usability
Trade-off
-
Analytics not as deep as enterprise systems
athenahealth
Best for: Clinics focused on ease of use + billing efficiency
Why It Performs Well
-
Extremely intuitive interface
-
Strong revenue cycle automation
-
Cloud-native reliability
Ideal Use Case
Clinics that want less IT management and faster staff onboarding.
AdvancedMD
Best for: Growing clinics with complex workflows
Key Strength
Highly configurable workflows for:
-
Multi-provider clinics
-
Specialty practices
-
Telemedicine-heavy models
Caution
Customization flexibility can increase setup time.
Kareo
Best for: Solo practitioners and small clinics
Why It Still Wins
-
Simple, clean UI
-
Affordable pricing
-
Minimal training required
Limitation
Not designed for complex analytics or large teams.
NextGen Healthcare
Best for: Specialty and ambulatory clinics
NextGen excels in:
-
Specialty-specific documentation
-
Ambulatory workflow optimization
-
Integrated analytics
2026 Trend Fit
Strong support for value-based care tracking.
CureMD
Best for: Multi-specialty and international clinics
Strengths
-
Modular architecture
-
Strong compliance updates
-
Flexible specialty support
EMR Comparison: Small Clinics vs Growing Practices
Clinic Type |
Best EMR Traits |
Recommended Systems |
|---|---|---|
Solo / Small |
Simplicity, low cost |
Kareo, eClinicalWorks |
Mid-Size |
Billing automation, telehealth |
athenahealth, AdvancedMD |
Large / Multi-Site |
Analytics, interoperability |
Epic, Oracle Health |
Key Features Clinics Should Prioritize in 2026
Instead of long feature lists, focus on impact areas:
Clinical Efficiency
-
AI documentation
-
Fast chart navigation
-
Voice input support
Revenue Protection
-
Real-time coding feedback
-
Denial prevention alerts
-
Integrated billing workflows
Patient Engagement
-
Easy-to-use portals
-
Mobile messaging
-
Telehealth continuity
Scalability
-
Ability to add providers easily
-
Multi-location support
-
API integrations
Challenges Clinics Still Face With EMRs
Even in 2026, EMRs are not plug-and-play.
Common pitfalls include:
-
Underestimating training time
-
Migrating messy legacy data
-
Choosing features over workflow fit
-
Ignoring staff feedback during selection
Expert Insight:
The best EMR is not the most advanced, it’s the one clinicians actually use correctly.
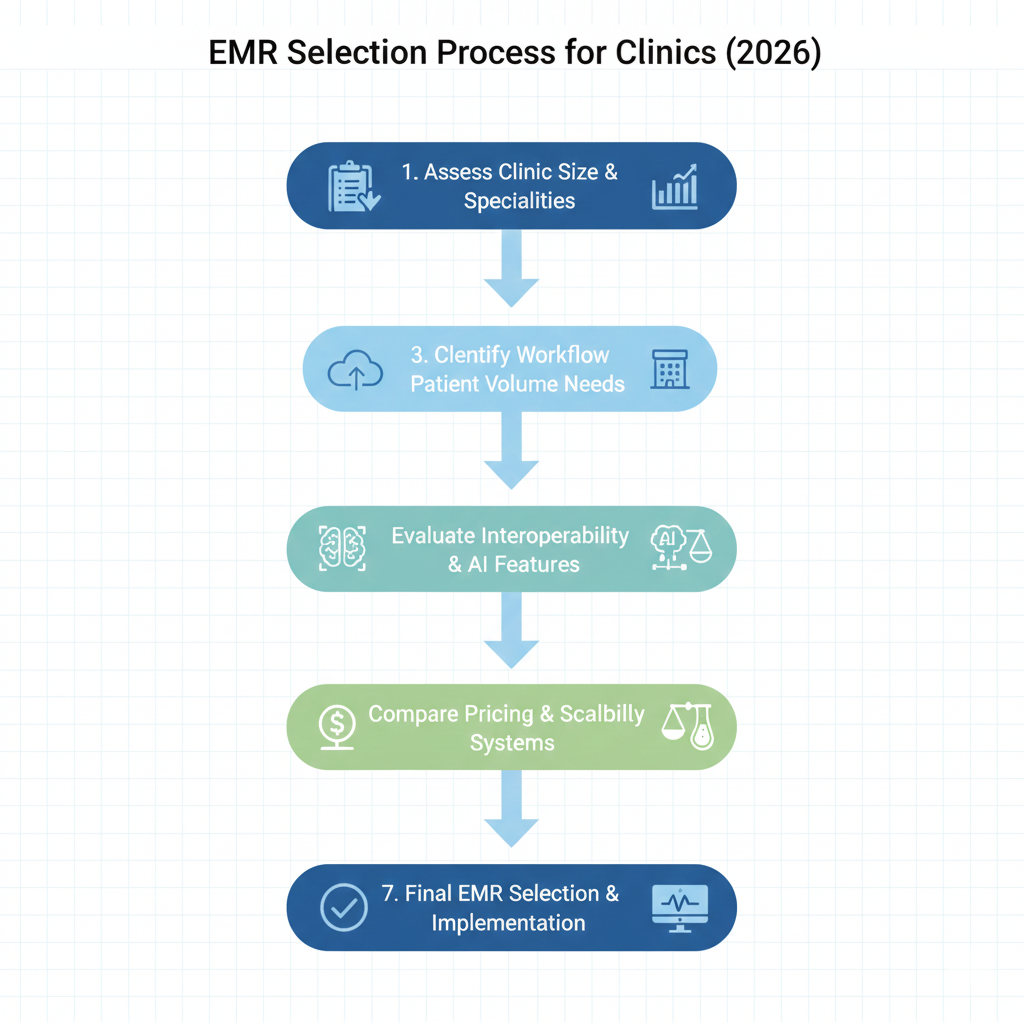
How to Choose the Right EMR (Decision Framework)
-
Map your current workflow pain points
-
Identify must-have vs nice-to-have features
-
Shortlist 2–3 vendors only
-
Request live demos using your real scenarios
-
Involve clinicians not just administrators
-
Evaluate long-term costs, not just onboarding fees
FAQs: EMR Systems for Clinics in 2026
Is AI documentation reliable?
Yes when reviewed. Clinics using AI still require clinician sign-off, but time savings are significant.
Are cloud EMRs safe?
Most breaches now occur from poor internal security practices, not cloud providers.
How long does implementation take?
Small clinics: 4–8 weeks
Large clinics: 3–6 months
Can EMRs support value-based care?
Modern systems increasingly include outcome tracking and reporting tools.
Final Thoughts: EMRs in 2026 Are Strategic Assets
In 2026, EMR systems are no longer just compliance tools. They shape:
-
How clinicians work
-
How clinics get paid
-
How patients experience care
The best EMR system for your clinic is one that reduces friction, protects revenue, and scales with confidence.
Clinics that treat EMR selection as a strategic decision not a software purchase will be the ones that thrive in the next decade of healthcare.